“DK Crush Bifurcation PCI”: Is it really the deal?
Zheng Feng CHEN, Huay Cheem TAN
National University Heart Centre, Singapore
Percutaneous coronary intervention (PCI) of coronary artery bifurcation disease is widely recognized to be challenging even for experienced interventionists. It is known to be associated with increased- short- and long-term adverse cardiac events, and reduced procedural success. The European Bifurcation Club (12th consensus document) recommends general adoption of the provisional stenting (PS) approach with bail-out side branch (SB) stenting if necessary as the primary strategy for most bifurcating lesions. It also states that upfront use of two stents may only be needed in very complex lesions with large calcified SB and SB ostial disease extending >5mm from the carina, and in bifurcations whose SB access is particularly challenging and should be secured by stenting once accessed. Should 2-stent bifurcation PCI be employed, high pressure kissing balloon inflation followed by proximal optimization is mandatory.
One of the most widely evaluated 2-stent bifurcation PCI technique in recent times, the ‘double-kissing’ (DK) crush method, was found to have favourable results in contemporary randomized clinical trials compared with provisional and other 2-stent bifurcating stenting techniques. This paper reviews the current literature surrounding this technique.
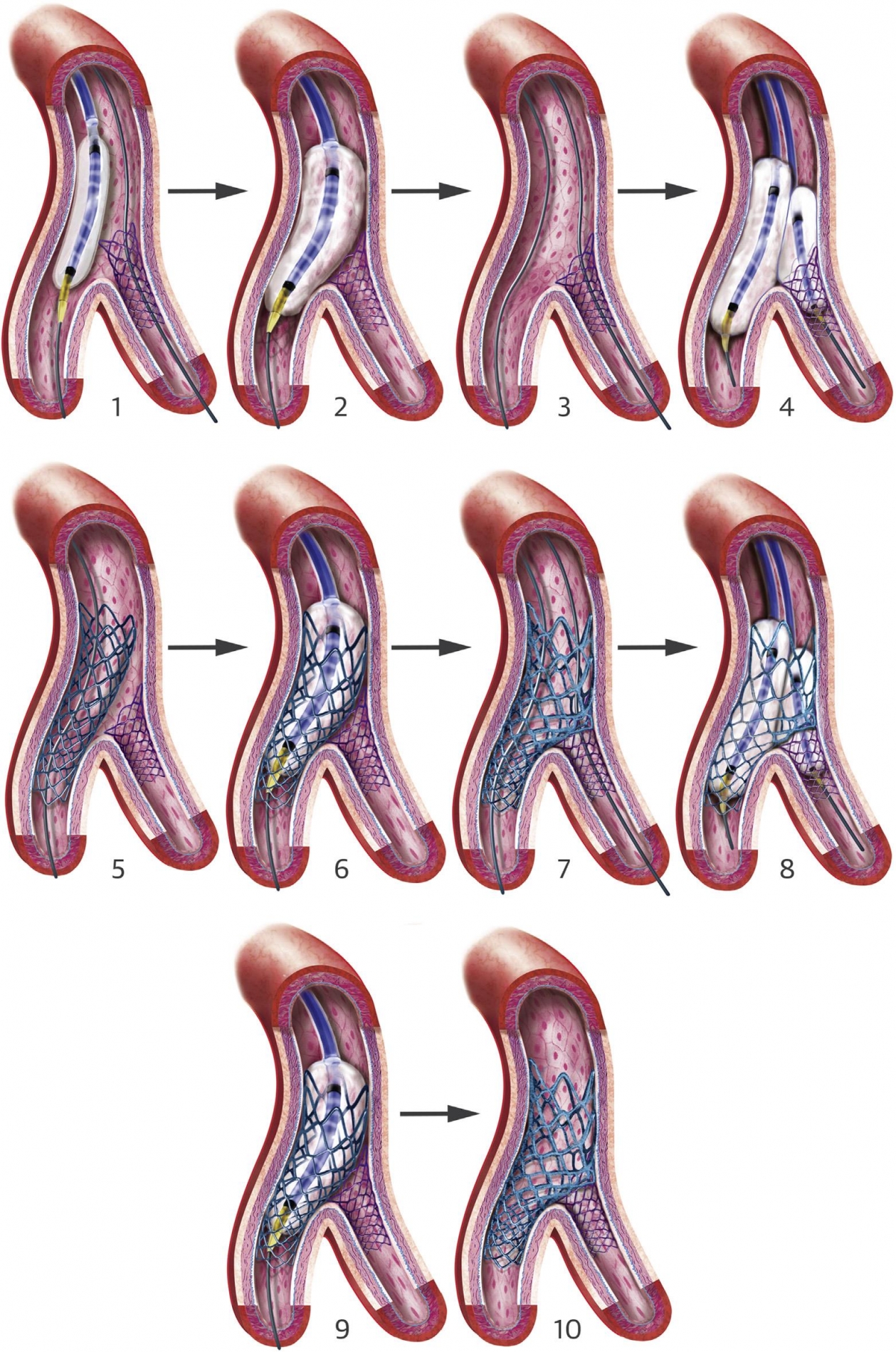
DK crush technique
The DK crush technique was developed by Zhang and Chen, and first described in 2005 (1). DK crush is performed with the following steps: 1) Stenting of the side branch (with 1 to 2 mm protrusion into the main vessel); 2) Balloon crush at main branch (MB); 3) Wiring of side branch (SB) through proximal cell of the crushed stent; 4) SB/MV high pressure alternative dilation and first kissing balloon inflation (KBI); 5) Stenting of MV after removal of the SB stent balloon and wire; 6) Proximal optimization technique (POT); 7) Re-wiring the SB through the proximal cell; 8) Second KBI; 9) Final re-POT and 10) Final result (Figure 1). The main difference between classic and DK crush is performing a first KBI after balloon crush of the implanted SB stent. This leaves only one layer of metal struts at the ostial SB with minimal distortion, and facilitates the second KBI after MV stenting. Unlike provisional SB stenting technique, re-crossing of the SB in DK crush should be carried out through the most proximal stent cell.
What has been studied for DK Crush
There have been many studies investigating the use of one- versus two stents in the treatment of non-left main (LM) bifurcation lesions, with most of the randomized trials showing no clear advantage of two-stent strategy over a provisional approach. A meta-analysis of these randomized trials show that both strategies result in similar outcomes in terms of target lesion revascularization (TLR), stent thrombosis, and cardiac death. In addition, periprocedural myocardial infarctions are significantly higher in complex versus simple strategies (NORDIC and BBC1 trials) (2-4). These results are markedly different if we focus on the DK crush technique alone.
Broadly, there have been a series of randomized controlled DKCRUSH trials beginning from I to VII evaluating this technique. Firstly, the DKCRUSH-I trial showed a significantly lower incidence of TLR with DK crush compared to classical crush treatment of non-LM bifurcation lesions at 1 year follow up. This is followed by DKCRUSH-II trial which showed reduced incidence of TLR and target vessel revascularization (TVR) with DK crush compared to PS for treatment of non-LM bifurcation disease.
Of particular importance is unprotected left main (ULM) true bifurcation disease, the so-called “big bifurcation”. This lesion subset should be viewed differently from other types of bifurcation disease, as the SB is the circumflex artery which typically accounts for significant myocardial territory. Therefore, it is usually not an option to lose the SB in distal ULM bifurcation disease stenting. The DKCRUSH-III trial investigated treatment of such ULM true bifurcation disease with DK crush versus Culotte, and found significant reduction of major adverse cardiac events (MACE) at 1-3 years follow up (5), along with reduction of stent thrombosis (ST) at 2-3 years follow up for patients treated with DK crush (6). A greater difference was seen during sub-group analysis of complex ULM lesions, with the rate of MACE being 51.5% in the Culotte group compared to 15.1% in the DK crush group. Bench testing of the Culotte technique has shown that a “napkin” or gap or metallic ridge is often present at the ostial SB. It is postulated that this leads to failure in complete coverage of the ostial SB which then results in increased in-stent restenosis (ISR), TLR and ST (7).
Another highly important trial is the DKCRUSH-V trial. This was a multi-centre trial randomizing 482 patients with ULM to DK crush or PS strategies. At one year follow up, DK crush had significantly lower rates of target lesion failure (TLF) (5.0% vs 10.7%, p=0.02), and lower rates of definite/probable ST (0.4% vs 3.3%, p=0.02). For patients with complex ULM bifurcation disease, the number needed to treat with DK crush to prevent TLF is a remarkably low number of 9. Complex ULM lesions were defined as being longer (>10mm SB lesion length), with more severe angiographic stenosis (>70% SB diameter stenosis), and at least two other high risk features such as severe calcification, intracoronary thrombus, multiple bifurcations, and acute or obtuse angulation. Patients undergoing PS had a numerically higher number of ISR compared to DK crush (8). At 3 year follow up, patients undergoing DK crush continue to have significantly lower rates of TLF (8.3%) compared to PS (16.9%). This is mostly driven by TLR and target vessel myocardial infarction (TVMI) (9). Notably at 3 years, the rate of definite/probable ST is also significantly lower in DK crush group compared to the PS group (0.4% vs 4.1%, p=0.006). ST was observed to occur more commonly in patients with higher SYNTAX score after PS and requiring rescue SB stenting. This suggests that an elective 2-stent approach like DK crush, instead of relying on bail-out stenting, is better in achieving optimal clinical outcomes for complex bifurcation lesions.
Certainly, we should consider coronary artery bypass grafting (CABG) for the more complex ULM lesions (high SYNTAX score > 32). However, in the EXCEL trial which showed non-inferiority of PCI compared to CABG revascularization of ULM disease, 25.1% had a high SYNTAX score, and 81% had distal LM bifurcation disease. The rates of stent thrombosis was 5.4% at 3 year follow for patients undergoing PCI in the EXCEL trial. This is comparable to patients undergoing provisional stenting in the DKCRUSH-V trial (5.8% at 3 year follow up). Although not directly comparable, the rates of ST for DK crush patients in DKCRUSH-V is remarkably lower at 2.5%, despite having a higher proportion of patients with a high SYNTAX score (37.9%). Perhaps, outcomes for patients with complex ULM disease undergoing PCI may be further optimized by choosing the appropriate bifurcation stenting strategy.
With regards to comparison between various 2-stent techniques, there is some evidence suggesting superiority of DK crush as per DKCRUSH-III. We are awaiting the results of the EBC MAIN study which will compare the various 2-stent techniques for LM bifurcation lesions against the provisional approach.
DKCRUSH-IV, VI, and VII are trials investigating the functional results of DK crush technique. In the DKCRUSH-IV trial, SB fractional flow reserve changes (FFR) were compared between patients undergoing DK crush versus PS for true bifurcation lesions. There was improved acute gain and late loss of SB FFR for patients in the DK crush group. Of note, final KBI was performed in all of those receiving DK crush, and significantly less for PS group (100% vs 83.8%, p<0.001) (10). DKCRUSH-VI investigated outcomes of FFR-guided versus angiography-guided provisional stenting of true bifurcation lesions. It showed no difference in MACE, TVR and ST rates between the groups (11). Finally, DKCRUSH-VII studied the FFR values during drug eluting stent (DES) implantation and found that a post-DES FFR of ≤0.88 predicted TVF, mostly driven by TVR and cardiac death. This was maintained through the 3-year follow up period. This suggests FFR is a potential marker of DES implantation success and can guide further post implantation stent optimization especially for high-stakes ULM intervention (12).
What is not known yet / limitations
The operators in the multicentre DKCRUSH trials are very experienced with more than >300 PCI/year for past 5 years and >20 LM PCI/year. Thus, the outstanding results seen for these complex lesions may not be fully replicable for all operators utilizing this advanced 2-stent technique. Of note, the already excellent results of DK crush in the DKCRUSH-V trial could be improved if the overall use of intravascular imaging was increased from the relatively low 42%. This is being studied in the on-going DKCRUSH-VIII trial comparing intravascular ultrasound guided versus angiographically guided ULM bifurcation lesions treated with DK crush technique.
Conclusion
There is mounting evidence that DK crush could be the technique of choice when a 2-stent strategy is chosen to treat bifurcation lesions. However, this precludes adopting a provisional approach. A better risk stratification and treatment algorithm based on the anatomical lesion complexities, such as using the DEFINITION criteria (13), may perhaps be the preferred approach in future. Taking it all together, DK crush appears to be the ‘real deal’ with the best clinical outcomes in true complex bifurcation disease requiring an up-front 2-stent strategy.
References
- Chen, S. L., Ye, F., Zhang, J. J. et al (2005). DK crush technique: Modified treatment of bifurcation lesions in coronary artery. Chinese Medical Journal, 118(20), 1746–1750.
- Steigen, T. K., Maeng, M., Wiseth, R. et al (2006). Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: The nordic bifurcation study. Circulation, 114(18), 1955–1961.
- Hildick-Smith, D., de Belder, A. J., Cooter, N. et al (2010). Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation, 121(10), 1235–1243.
- Behan, M. W., Holm, N. R., Curzen, N. P. et al (2011). Simple or complex stenting for bifurcation coronary lesions : A patient-level pooled-analysis of the nordic bifurcation study and the british bifurcation coronary study. Circulation: Cardiovascular Interventions, 4(1), 57–64.
- Chen, S. L., Xu, B., Han, Y. L. et al (2013). Comparison of double kissing crush versus culotte stenting for unprotected distal left main bifurcation lesions: Results from a multicenter, randomized, prospective DKCRUSH-III study. Journal of the American College of Cardiology, 61(14), 1482–1488.
- Chen, S. L., Xu, B., Han, Y. L. et al (2015). Clinical Outcome After DK Crush Versus Culotte Stenting of Distal Left Main Bifurcation Lesions: The 3-Year Follow-Up Results of the DKCRUSH-III Study. JACC: Cardiovascular Interventions, 8(10), 1335–1342.
- Murasato, Y., Hikichi, Y., & Horiuchi, M. (2009). Examination of stent deformation and gap formation after complex stenting of left main coronary artery bifurcations using microfocus computed tomography. Journal of Interventional Cardiology, 22(2), 135–144.
- Chen, S. L., Zhang, J. J., Han, Y. et al (2017). Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. Journal of the American College of Cardiology, 70(21), 2605–2617.
- Chen, X., Li, X., Zhang, J. J. et al (2019). 3-Year Outcomes of the DKCRUSH-V Trial Comparing DK Crush With Provisional Stenting for Left Main Bifurcation Lesions. JACC: Cardiovascular Interventions, 12(19), 1927–1937.
- Ye, F., Chen, S. L., Zhang, J. J. et al (2012). Hemodynamic changes of fractional flow reserve after double kissing crush and provisional stenting technique for true bifurcation lesions. Chinese Medical Journal, 125(15), 2658–2662.
- Chen, S.-L., Ye, F., Zhang, J.-J. et al (2015). Randomized Comparison of FFR-Guided and Angiography-Guided Provisional Stenting of True Coronary Bifurcation Lesions. JACC: Cardiovascular Interventions, 8(4), 536–546.
- Li, S. J., Ge, Z., Kan, J. et al (2017). Cutoff Value and Long-Term Prediction of Clinical Events by FFR Measured Immediately After Implantation of a Drug-Eluting Stent in Patients With Coronary Artery Disease: 1- to 3-Year Results From the DKCRUSH VII Registry Study. JACC: Cardiovascular Interventions, 10(10), 986–995.
- Chen, S. L., Sheiban I, Xu, B. et al (2014). Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv 2014;7:1266–76.
